Iron Deficiency: How to Master Diagnosis and Treatment for Your Complex Admitted Patients
Detailed discussion of lab cutoffs for iron deficiency in complex patients with a focus on oral and IV treatment options.

This post outlines lab cutoffs for iron deficiency in healthy patients and those with heart failure, ongoing inflammation, or chronic kidney disease. Oral and IV treatment options are reviewed.
Does your patient have iron deficiency?
The most useful labs are ferritin and transferrin saturation percent (TSAT). The TSAT is usually reported, but if not, it can be calculated by dividing the iron level by the total iron binding capacity (TIBC).
Iron deficiency is indicated by the following:
- Almost ANY patient -> Ferritin less than 30 mg/dL
- Active inflammation ->TSAT <20% and ferritin less than 100 mg/dL.
- CKD -> TSAT <20% and ferritin less than 200 mg/dL.
- CHF1–3 -> ferritin <100 mg/dL OR
-> ferritin 100-300 mg/dL + TSAT <20% - Clinical and lab improvement after trial of iron replacement
If the patient has anemia associated with the iron deficiency, they will often also have RBC indicators of low MCV, high RDW, low MCHC, and low reticulocyte count. They may also have symptoms such as fatigue, restless leg syndrome, PICA, or dyspnea.
Soluble transferrin receptor is sometimes used to help decide if a patient has anemia of inflammation OR anemia of inflammation + iron deficiency.
Iron deficiency and treatment for patients on dialysis is somewhat different because patients lose iron with every run of hemodialysis.4 There is variation among nephrologists regarding the ferritin and TSAT cutoffs that indicate iron deficiency or benefit from treatment. A recent trial used a ferritin of 400 mg/dL and TSAT of 30% for cutoffs.
Iron Deficiency is a SYMPTOM that demands evaluation
Healthy patients who eat a normal diet don't have iron deficiency. If this new finding is identified, it begs the question as to what is causing it. Does the patient have some source of ongoing bleeding or a malabsorption syndrome? Consider the following:
- Age-appropriate cancer screening
- Colonoscopy and EGD if no other cause is identified
- Inflammatory bowel disease
- Celiac disease
- Menorrhagia
- Hematuria
- Diffuse alveolar hemorrhage
- Lice
- H. Pylori
- Autoimmune gastritis
- Use of proton pump inhibitor (PPI)
Indications and contraindications for treatment
Any patient with iron deficiency should be treated (eventually).
The main reason to postpone treatment is if the patient has a severe uncontrolled bacterial infection. Iron deficiency treatment has been associated with increased risk of infection.5,6 The data on this are weak, but if the patient doesn't have a life-threatening anemia or hemodynamic instability, then why risk it? If a patient has source control, is on antibiotics, and is clinically improving, then it's not unreasonable to go ahead and initiate iron replacement.
IV vs oral iron
Oral iron is poorly tolerated even when dosed properly (one tablet every other day).7 If the patient is admitted and has IV access, then just use IV iron. This would be doubly true if the patient is symptomatic from their anemia.
IV Iron is especially indicated for patients who are not going to absorb oral iron. For example, consider the following conditions:
- Inflammatory bowel disease
- Celiac disease
- Small bowel resection
- Gastric bypass surgeries
- Demonstrated failure of oral iron response
Furthermore, patients with ongoing inflammation poorly absorb iron from the gut.8 This happens because hepcidin down-regulates the ferroprotein on enterocytes.9,10 The iron just isn't absorbed well regardless of their gut health and dietary intake.
IV iron dosing and formulation
There are two common ways to dose IV iron. Either calculate the iron deficit and replete to that amount OR empirically treat with 1 gram of IV iron.11
Option 1 (preferred): Use the Ganzoni equation to calculate the patient's total iron deficit and then replete that amount. Typically, the deficit will be 500-1500 mg.
Total iron dose = 2.4 * weight * (target Hb - actual Hb) + IronStoresIron stores = 10-15 mg/kg IBW
Option 2: empirically treat with 1 gram of IV Iron
Pick an iron formulation and give one dose per day until the deficit is repleted.
High molecular weight Iron dextran is bad: 1 in 100 patients exposed suffer severe life-threatening anaphylaxis. To allow usage, patients were typically pre-treated with steroids and antihistamines. Low molecular weight iron dextran has a lower anaphylaxis risk, and if a test dose is given, then it’s not unreasonable to use.12
Otherwise, use whichever formulation your hospital has available. Severe adverse effects are extremely rare with more recent formulations.12,13 The benefit of curing iron deficiency certainly outweighs the risk. Some examples of formulations that may be available include:
- Iron sucrose (Venofer) - 100-300 mg per dose
- Iron gluconate (Ferrlecit) - 125 mg or 250 mg per dose
There are other formulations typically used in dialysis centers that allow higher mg per dose, but they are more expensive and are not commonly used were I practice.
Oral iron dosing and formulation
Decide on an iron deficit and treat with ferric gluconate one tablet every other day. Recent data suggest that this strategy is non-inferior to more aggressive dosing and allows for improved tolerance/compliance.7 The underlying physiology is thought to reflect hepcidin increases after an iron dose reducing the absorption of subsequent dosing.
Absorption of oral iron is variable. The duration of treatment should be based on the iron deficit and improvement in the ferritin, TSAT, and the RBC indices. It wouldn't be unreasonable to recheck labs after a few months of treatment.
Clinical pearls
One time blood transfusion does not significantly affect iron studies within 48 to 72 hours.14 Though this is not much data on this topic. Some older small studies (10-30 patients) found the opposite conclusion.15,16
Iron dextran is the original IV iron formulation. It has a higher risk of anaphylaxis (1-2%) and requires a test dose before administering the full dose. Newer IV iron formulations are extremely safe and adverse effects are not common. Furthermore, they don’t require a test dose.
The evidence is not robust for ferritin and TSAT cutoffs in patients with inflammation, CKD, and heart failure; they will likely slightly be evolving over time as better data are reported.
Treating iron deficiency in patients admitted with acute decompensated heart failure reduces readmission for heart failure.1
Examples
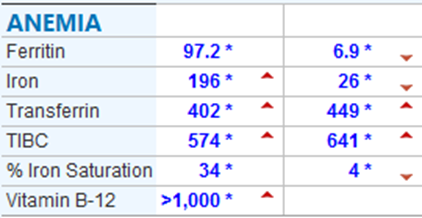
This patient presented with fatigue and anemia in the setting of ongoing blood loss. Their initial iron studies showed a ferritin of 6.9 and a TSAT of 4. This is the quintessential presentation of iron deficiency. The image below showed iron studies at followup (left column) and initial iron studies.
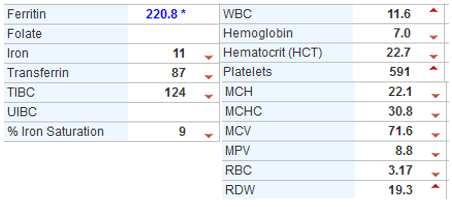
This patient had multiple wounds and osteomyelitis. The iron studies and CBC together indicate likely anemia of chronic deficiency AND iron deficiency.
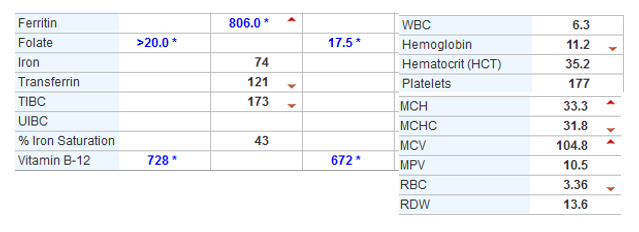
This patient had acute inflammation and end stage renal disease and had a macrocytic anemia that didn't have a clear etiology; but they did not have iron deficiency.
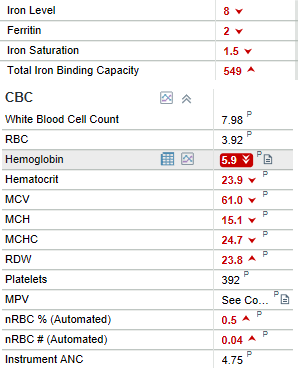
This patient presented with dizziness and chest pain. They had large uterine fibroids and poor access to care. She had severe iron deficiency anemia.
References
1. Graham FJ, Pellicori P, Ford I, Petrie MC, Kalra PR, Cleland JGF. Intravenous iron for heart failure with evidence of iron deficiency: a meta-analysis of randomised trials. Clin Res Cardiol. 2021;110(8):1299-1307. doi:10.1007/s00392-021-01837-8
2. Ponikowski P, Kirwan BA, Anker SD, et al. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. The Lancet. 2020;396(10266):1895-1904. doi:10.1016/S0140-6736(20)32339-4
3. Grote Beverborg N, Klip IjT, Meijers WC, et al. Definition of Iron Deficiency Based on the Gold Standard of Bone Marrow Iron Staining in Heart Failure Patients. Circ Heart Fail. 2018;11(2):e004519. doi:10.1161/CIRCHEARTFAILURE.117.004519
4. Macdougall IC, White C, Anker SD, et al. Intravenous Iron in Patients Undergoing Maintenance Hemodialysis. N Engl J Med. 2019;380(5):447-458. doi:10.1056/NEJMoa1810742
5. Shah AA, Donovan K, Seeley C, et al. Risk of Infection Associated With Administration of Intravenous Iron: A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4(11):e2133935. doi:10.1001/jamanetworkopen.2021.33935
6. Cross JH, Bradbury RS, Fulford AJ, et al. Oral iron acutely elevates bacterial growth in human serum. Sci Rep. 2015;5(1):16670. doi:10.1038/srep16670
7. Stoffel NU, Cercamondi CI, Brittenham G, et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials. Lancet Haematol. 2017;4(11):e524-e533. doi:10.1016/S2352-3026(17)30182-5
8. McSorley ST, Jones I, McMillan DC, Talwar D. Quantitative data on the magnitude of the systemic inflammatory response and its relationship with serum measures of iron status. Transl Res. 2016;176:119-126. doi:10.1016/j.trsl.2016.05.004
9. Ganz T, Nemeth E. Iron Balance and the Role of Hepcidin in Chronic Kidney Disease. Semin Nephrol. 2016;36(2):87-93. doi:10.1016/j.semnephrol.2016.02.001
10. Ludwiczek S, Aigner E, Theurl I, Weiss G. Cytokine-mediated regulation of iron transport in human monocytic cells. Blood. 2003;101(10):4148-4154. doi:10.1182/blood-2002-08-2459
11. Koch TA, Myers J, Goodnough LT. Intravenous Iron Therapy in Patients with Iron Deficiency Anemia: Dosing Considerations. Anemia. 2015;2015:1-10. doi:10.1155/2015/763576
12. Wong L, Smith S, Gilstrop M, et al. Safety and efficacy of rapid (1,000 mg in 1 hr) intravenous iron dextran for treatment of maternal iron deficient anemia of pregnancy: Intravenous Iron for Maternal Iron Deficient Anemia. Am J Hematol. 2016;91(6):590-593. doi:10.1002/ajh.24361
13. Faich G, Strobos J. Sodium ferric gluconate complex in sucrose: Safer intravenous iron therapy than iron dextrans. Am J Kidney Dis. 1999;33(3):464-470. doi:10.1016/S0272-6386(99)70183-6
14. Froissart A, Rossi B, Ranque B, et al. Effect of a Red Blood Cell Transfusion on Biological Markers Used to Determine the Cause of Anemia: A Prospective Study. Am J Med. 2018;131(3):319-322. doi:10.1016/j.amjmed.2017.10.005
15. Saxena S, Shulman I. The effect of blood transfusion on serum ferritin level. Transfusion (Paris). 1993;33(10):883-884. doi:10.1046/j.1537-2995.1993.331094054628.x
16. Saxena S, Shulman IA, Johnson C. Effect of blood transfusion on serum iron and transferrin saturation. Arch Pathol Lab Med. 1993;117(6):622-624.
Disclaimer
All information in this post is for educational use only and is not a replacement for formal medical education.